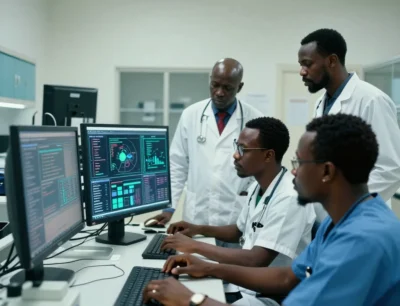
AI-Powered Clinical Trials: A Game Changer for Global Health Access
AI is helping drugmakers speed up clinical trials and regulatory submissions—cutting delays and getting treatments to
Notice: Test mode is enabled. While in test mode no live donations are processed.
AI is helping drugmakers speed up clinical trials and regulatory submissions—cutting delays and getting treatments to

Gates and OpenAI launch Horizon1000 to bring AI to 1,000 African clinics — expanding healthcare access through locally

AI is boosting vaccine rates in rural India. See how smart tracking tech in Fatehpur raised child coverage to 95%—a mo
