AI in the Pharmacy: Faster Refills, Smarter Systems
Utah tests AI to renew prescriptions without doctors. A bold step in healthcare automation with real-world patients and
Notice: Test mode is enabled. While in test mode no live donations are processed.

Utah tests AI to renew prescriptions without doctors. A bold step in healthcare automation with real-world patients and
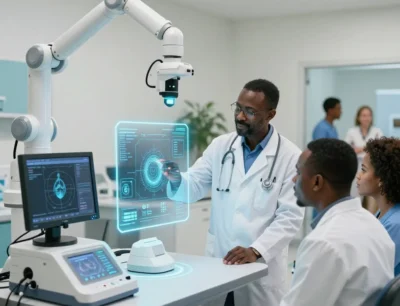
India’s first government-run AI clinic opens in Noida — transforming public healthcare with AI diagnostics, genomics

This winter, AI is helping the NHS forecast demand, reduce A&E wait times, and free up doctors to focus on patients—no
